Of course you can dress any which way you like. But we know that some of you worry that you look too young, or you feel that you may be trying too hard to stay young. We’ve also been getting questions on how to avoid appearing older than you are. So here are some of our guidelines on how to dress after 40.
Please note that these are just GENERAL guidelines and some of our own personal preferences. They certainly don’t apply to everyone.
However, we do believe in dressing to your strengths and taking your body shape and style personality into account. So, if you would like to have some guidelines on how to dress after 40, then you can find them below.
How can I look chic at 40?
Take a look at our top style tips (below) to find the most stylish outfits for you. It’s all about getting your essentials right, thinking timeless rather than trendy, and working out what is most flattering for your body type.

Cathy @themiddlepageblog above (read her style interview here)
She is wearings a top and a bomber jacket from Anthropologie and a pair of cargo jeans from EVEREVE (another option here). Check out this similar bag (another option here), booties, belt and sunglasses to complete the look.
How to reinvent your look at 40?
Whether you’re thinking about adding a little extra oomph to your existing looks or you want to completely transform your style, the guidelines below will give you the inspiration you need.
HOW TO DRESS AFTER 40 – WHAT ARE SOME OF THE THINGS YOU SHOULD AVOID?
Below are a few general guidelines on what to avoid doing in terms of style after 40, style over 50 or any age above.
1. DON’T BUY CLOTHES THAT DO NOT FLATTER YOU, EVEN IF THEY ARE ON TREND THIS SEASON.
You may be tempted by a new trend but, when thinking about how to dress after 40, it’s wise to be picky. Only choose those that suit your personality and your your body type. You can find guides on dressing all the different body types in these articles:

Where to shop the best midi dresses: COS, Nordstrom. Shoes: Fly London (similar). Bag: similar
2. TRY NOT TO BE TOO MATCHY-MATCHY OR TOO POLISHED
It’s nice to mix things up and be a bit more playful. A two-piece suit will quickly look old. Better to mix that jacket with another skirt or pants and look effortlessly chic. You could wear your blazer with jeans, for example, like in the look below.

J.Crew Linen Blend Helena Blazer – Boden Short Sleeve Wrap Top – PAIGE Leenah Wide-Leg Jeans – Vagabond Shoemakers Cassie Leather Booties – Tory Burch Small Ella Bio Tote – Balenciaga Loop Earrings
3. AVOID BUYING FABRICS THAT LOOK CHEAP (OR ARE CHEAP AND POORLY MADE) AS THEY ARE USUALLY NOT FLATTERING OR WILL NOT LAST
As a young woman, you may have looked cute in a flimsy, poorly made t-shirt but as a woman over 40, you need something with a bit more substance.
You can see some characteristics of fabrics here. We also have a list of recommended shops here. Best to buy only the clothes that you love and that have a chance to last.
Look for beautiful natural fabrics like silk, cotton, linen and cashmere and you will enjoy them for years to come. Think about your purchase in terms of cost per wear rather than initial price.
Avoid fabrics that don’t drape well or cling.

Eileen Fisher Classic Collar Easy Shirt – Favorite Daughter The Agnes Pleat Front Wide Leg Pants – Franco Sarto Tracy Slingback Pumps – Tory Burch Small Ella Bio Tote – Tory Burch Kira Imitation Pearl Layered Necklace
4. WEARING TIGHT AND TIGHT TOGETHER
Of course there are many exceptions but in general tighter items like leggings look better when they are combined with wide pieces like a tunic or wider shirt.
That also applies to skirts. Aim to have either a tight skirt with a loser top or vice versa. You could wear a loose, tunic style shirt with leggings or your skinny jeans. Or choose wide pants and a tighter-fitting top.

Akris Punto Square-Neck Blouse – Alice + Olivia Pompey High-Rise Pleat Trousers – MICHAEL Michael Kors Townsend Small Top Zip Convertible Crossbody – Franco Sarto Tracy Slingback Pumps – Balenciaga Loop Earrings
For more style inspiration on how to wear your pair of loafers, see our article on the best loafers for women over 40.

Tanasha @letsrecreatethelook above mixes fabrics with her jersey top and leather look pants.
Steal her look with this similar top, pants (another option here), pumps, handbag, earrings and headband.
5. CHECK OUR GUIDELINES FOR THE FOLLOWING ITEMS:
- Shorts: choose the ones that are right for you – Find out how to wear shorts
- Leggings: find out how to wear leggings the right way
- Mini dresses – we prefer these as tops for women over 40. Have a look at how to wear short dress with pants.
- Jeans – check out our recommendations how to wear jeans over 40
- Wide pants – these can look fabulous when you keep the right proportions in mind – check our guidelines on how to wear wide pants
- Blazers – check our guidelines on how to fit a blazer
- Skirts: you will like our guidelines on the best skirt for your body type
DRESSING OVER 40: WHAT ARE SOME OF THE THINGS YOU SHOULD DO MORE OF?
1. KNOW YOUR STYLE!
Nothing is more important than dressing in a way that pleases and represents you. There’s no such thing as one style of “fashion for older women” that suits everyone.
If you know your style and understand your body you can break any of the rules or add items from the ‘don’t list’ as you please. My style guide will help with that.
Doing our style personality quiz will also give you a better idea of your style.
My style is comfortable, asymmetric, colorful and minimal. I identify the most with architectural and eurochic style personalties.

Dress from COS. Other options here and here
2. DETERMINE THE WARDROBE ESSENTIALS THAT ARE UNIQUE TO YOUR STYLE
Not everyone will have the same wardrobe essentials. This will depend on your lifestyle and your style personality.
But having a collection of wardrobe essentials in your closet will make dressing every day so much easier – and more stylish.
Personally, I love to have plenty of asymmetrical items in my closet.
3. HAVE MORE LASTING HIGH QUALITY ITEMS IN YOUR WARDROBE
These vary for each style personality but some important classics are:
- A white button down shirt. Check our tips on how to wear a white shirt
- A long coat (could be a trench coat). Check out tips on how to choose a coat.
- A beautiful dress that fits you perfectly. Don’t automatically go for a little black dress. Many women over 40 will actually look better (and slimmer) in a colorful dress. – you may like to get a dress with sleeves
- Well fitted long pants. Check out what shoes to wear with different styles of pants
- A well fitted blazer.
- A good pair of dark denim jeans that fit you well. Boot cut or straight leg is usually the most flattering style. Check all our tips on wearings jeans.

Reformation Garrett Cashmere Cropped Turtleneck Sweater – Eileen Fisher Classic Collar Easy Shirt – PAIGE Leenah Wide-Leg Jeans – Paul Green Teddy Flats – Tory Burch Small Ella Bio Tote – Deepa Gurnani Aria Oval Crystal Stud Earrings

Jona @the50plusgirl above wears her trench coat with a leopard print shirt.
Check out this similar sequin top, trench coat, skirt (other options here and here), pumps, handbag (another option here), necklace and sunglasses.
4. LOOK EFFORTLESSLY CHIC
You know how they say that French women look so effortlessly chic. That’s because they appear not to have spent a lot of time on their clothes, yet look amazing.
However, an effortlessly chic look takes time so you want to think carefully about the right combination of items, shoes and accessories.
On the other hand, you don’t want to overdo your look. Don’t add too many accessories, don’t be too matchy-matchy and find the right combination of high end / low end and casual and chic.
Want to know how to create that effortlessly chic look take a look at our article on French style. Or go even more sophisticated and opt for Italian style.
5. Fashion over 40: MIX AND MATCH DESIGNER ITEMS WITH NON-DESIGNER ONES
Even if you have a closet of designer items, it’s a great idea to mix a few designer pieces with high street options. That way, you can affordably add some on-trend clothes and accessories to your closet while keeping your timeless, designer classics part of your outfits too.

Apparis Aria Duster Cardigan – Tory Burch Printed T-Monogram Jersey Tee – Hudson Jeans Barbara Coated Straight-Leg Jeans – COACH Jolene Loafer – Rebecca Minkoff Julian Backpack – Swarovski Stilla Crystal Hoop Drop Earrings

Rita @ritapalazzi above (read her style interview here) chooses a colorful designer bag to match the print in her t-shirt.
Get her look with this similar top (another option here), jeans, handbag (another option here), pumps (another option here) and sunglasses.
6. CHOOSE A SKIRT OR DRESS LENGTH THAT’S RIGHT FOR YOU
For many women dresses and skirts that are just above or on top of the knee are a great length for women over 40. Right now longer dresses are very much on trend as well and can be a great style for older women to choose.
Petite women may want to go a bit shorter with their skirt lengths to get the 1/3 – 2/3 silhoutte. Find out more about this rule of thirds in our article on how to wear capris.
Adding a moto jacket to your dress like in the look below is a great way to mix formal and casual in your outfit.

Cinq à Sept Zoe Biker Jacket – Nordstrom Satin Midi Shirtdress – Bernardo Hammond Over-The-Knee Boots – COS The Halo Leather Tote – Deepa Gurnani Aria Oval Crystal Stud Earrings
For more inspiration, see this article on the perfect skirt length for women over 40.
7. Don’t neglect your casual wardrobe
It’s easy to be attracted to evening wear on the store rails or online. However, it’s likely that you will actually wear your casual outfits much more.
So, don’t neglect your day-to-day wardrobe. You could choose a drapey cardigan to add style and warmth to a simple jeans and t-shirt outfit. Or add a blazer to casual wear to elevate your look. Look for shirts and tops in beautiful materials and add some texture to your outfits.
Check out some recent articles on casual style:

Sam Edelman Hooded Parka Coat – Reiss Lorey Colorblocked Silk Satin Shirt – – Hudson Jeans Barbara Coated Straight-Leg Jeans – Cole Haan Grandpro Topspin Sneakers – Rebecca Minkoff Julian Backpack – Swarovski Stilla Crystal Hoop Drop Earrings

Adaline @sdmomstyles above wears a long cardigan with her tracksuit pants and sneakers.
Recreate her outfit with this similar shirt, coat, joggers, sneakers and shoulder bag.
8. MIX YOUR OWN STYLE WITH A TREND YOU LIKE
Keep updated with the fashion trends and make sure you have a few current items in your wardrobe. For the best style over 40, only pick those trends that work for you!

Tanya Taylor Carlita Striped Twist Top – Veronica Beard Saul Cargo Pants – Cole Haan Grandpro Topspin Sneakers – MICHAEL Michael Kors Townsend Small Top Zip Convertible Crossbody – Balenciaga Loop Earrings
9. Have fun with color
Don’t be afraid of color. Women over 40 benefit from adding more color to their looks. Not only will it enhance your complexion, you also add a bit of pizazz to your style.
Your may like to take inspiration from our color guides.
Choose a bright, modern print blouse and you can wear with your jeans, or dress up with a skirt or by tucking into wide leg pants.

NIC+ZOE Petal Splash Long-Sleeve Blouse – Modegal Satin Midi Skirt – Stuart Weitzman Eva Pumps – Cult Gaia Caldera Metallic Clutch Bag – Balenciaga Loop Earrings

Similar top, skirt, sandals, bag, necklace and earrings
10. PLAY WITH ACCESSORIES
Wear accessories like belts, jewelry and scarves. They can make a real difference to your outfit. You could add a statement necklace to a block color top or dress.

Read our article on how to wear accessories.
11. WEAR HIP AND CURRENT SHOES
These add an instant young and hip vibe to your outfits.
Make sure to choose shoes that you are able to walk in. Mid-high heels can look fabulous. Gold or silver shoes will go with everything.

Kenneth Cole Reaction Nessa Textured Sandals
If you need more support I have a great list of arch support shoes.
12. Invest in a great pair of flattering jeans
Your jeans can be the mainstay of your closet as they go with so many other things, and can be dressed up or down.
Opt for a style which flatters your figure rather than the latest on-trend jeans shape. Bootcut jeans are back on trend, and tend to suit most body shapes. Classic blue or black will be truly timeless, or add a pop of color with your jeans.

Mango Belted Coat – Eileen Fisher Classic Collar Easy Shirt – FRAME Le Slim Palazzo Jeans – Stuart Weitzman Eva Pumps – COS The Halo Leather Tote – Swarovski Stilla Crystal Hoop Drop Earrings
Also, take a look at the most flattering jeans for every body type.
13. OPTIONAL: USE SHAPEWEAR
If you want to hide some of the bulges, then shapewear definitely helps. I personally only wear it on special occasions.
If you don’t like shapewear, then learning how to skilfully hide with the right clothes will be preferable, like these tips in my article on how to hide your belly.

SKIMS Body Plunge Mid-Thigh Bodysuit
14. WEAR A GOOD BRA
Make sure you wear a good bra and invisible undergarments. A great bra will make sure that there is a clear distance between your chest and your tummy!

Hanro Allure Strapless Convertible T-Shirt Bra
More info in my article on how to find the perfect bra.
15. WEAR WHAT MAKES YOU FEEL AMAZING

Similar dress, strappy sandals, necklace and sunglasses.
The most important style “rule” of all is to wear what makes you feel confident. That way, you’ll have a spring in your step and you’ll be ready for whatever the day brings. So, choose what makes you feel great when you look in the mirror before you head out.
WEAR WHAT FEELS RIGHT TO YOU!
I want to emphasize again that these tips on how to dress after 40 are not set in stone and it’s up to you to decide what works best for you. But if you want to look young and hip, then these guidelines can certainly help.
The more you understand your body and your style, the more you can break these rules as you please.
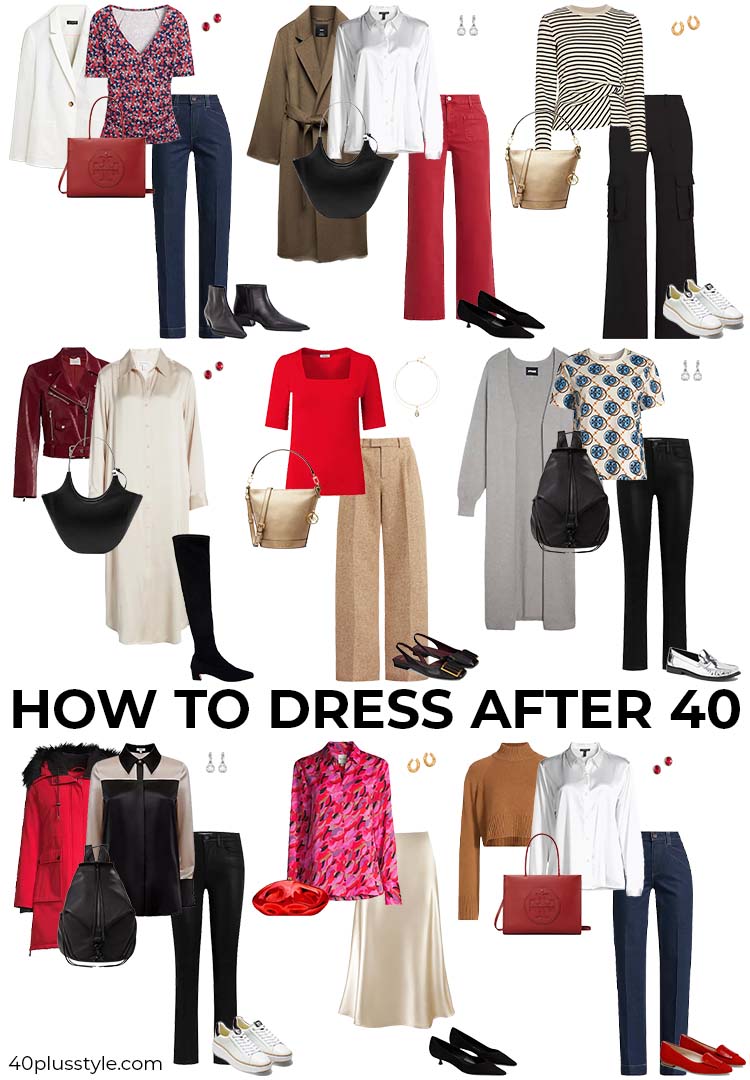
Below is a capsule wardrobe we created that you can mix and match to create lots of different outfits. You could wear the stripe top with the red jeans, for example, or the long cardigan with the shirtdress. You can wear the bright colors together or create an all-neutral outfit.
How do i look trendy in my 40s?
If you’re thinking about how to look trendy in your 40s, the best piece of advice we can give is ‘don’t’. Don’t think about looking trendy. Think about developing your own style. You can always add a trend or two to update your outfits, but don’t base your entire outfit around being on-trend.
What should a 40 year old woman wear?
As we’ve been discussing, you should wear whatever makes you feel most confident. There are no hard and fast ‘rules’. Our guidelines are here to help and inspire you to find your own unique style.
shop the items above here:
For all my best tips on how to dress after 40 and a complete style course that will get you looking stylish in no time, I highly recommend my style course.
If you have any further tips then I would love to hear them. Enjoy!
What are your tips on how to dress after 40? Share them below.
Continue reading:
- How To Dress Over 40 – My Top 10 Tips
- How To Determine Your Body Shape
- How To Build Self Confidence And Believe In Yourself – The One Thing That Actually Works
LIKE THIS POST on how to dress after 40? SHARE IT ON PINTEREST!


Sylvia is 40+style’s editor-in-chief and has been helping women find their unique style since 2011. An alumni of the School of Color and Design, she is devoted to empowering women of any age to look and feel their best. Read more about Sylvia and 40+style on this page.
Want to get more articles from 40+style in your inbox, subscribe here.
You can also connect with 40+style on Facebook, Instagram or Pinterest.
Support 40+style by using the links in our articles to shop. As an associate for Amazon and many other brands, we receive a small commission (at no cost to you) on qualifying purchases which enables us to keep creating amazing free content for you. Thanks!


Hi, I’m 47 and have just ordered myself 2 midi dresses in a ditsy floral pattern, I like this style of dress because they are still flattering and classy. ive sorted through my wardrobe and got rid of a lot of short dresses and skirts, although I’m young looking and slim I now want a more classic look.its time to hang the boots up on mini dresses for me.
What a great list!! I especially appreciate the one about figuring out the dress length, however I think the fulness of the skirt might have some impact.
You look great in the the dress that makes you feel great :). Your shoes really capture the feeling of the dress!!
As with anything in life, you take the best and move on. So do the same here. Learn from the tips given and apply the styling solutions. If it doesn’t fit your looks, shape, size or life style, then just move on.
Women of all shapes and sizes look for styling ideas like the ones shared here. Give us a break with the self-serving criticisms. Enough.
Why do these posts seem to automatically assume that if you’re over 40 you are heavy set or have bulges?
Anyway, I’m 43, but I look quite young and have yet to get wrinkles or grey hair. I’m thin and fit and my problem is that people guess my age as young as early to mid 20’s. This kinda stinks because men my age view me as too young for them. I dress classy and fashionable, but I want to look closer to my age! I don’t know what to do! I’m so frustrated!
I’m not assuming anything as I write articles for women of all shapes and sizes. I just know that it’s a reality for a majority of my readers so I’m also speaking to them. An unusual problem to have as I usually hear the opposite (as men often prefer younger women). What I can suggest though is to opt for more classic clothes. These will usually lead you to appear older.
Hello, I was just wondering what your thoughts on dressing closer to the age I actually look? I’m about to turn 40 and most people think I’m early 30’s. One thing I do know is I love my jeans and band t-shirts and will very likely keep those around to wear sometimes til I die, haha
You have to dress for what makes YOU happy There is no need to ditch the jeans and t-shirts at any age. Always stay true to who you are and you can wear anything.
Hi!
do the same rules apply to 50+ women too?
rgds
Please note these are not ‘rules’, just guidelines. Yes these are good for all women over 40 🙂
It seems like everyone commenting on this “Women over 40” website is skinny and using this forum to brag how awesome/hot they look. What about the woman in her early 50’s who is dealing with perimenopause and the accompanying 40 lbs that have settled mainly in my gut and is resistant to diet and exercise? I feel embarrassed to go out and only wear black when I do. The same outfit over and over, literally. I feel like a big fat pig, and would love any advice on how to dress at this weight/stage of life.
Actually we have lots of women with curves in this community. Most of my readers deal with bigger bellies and increased weight. You may find this article on that topic interesting. https://40plusstyle.com/how-to-hide-your-belly/ Wearing all black is not a good option though. You may feel that this hides your belly better but you end up looking drained and perhaps also insecure. It’s much better to play with color, texture and layers. You are still beautiful so it’s also really important not to use those awful words you used to describe yourself. You can be bigger and gorgeous and if you learn how to dress for your new body and show confidence, you will be just as beautiful as before. You may like to join my free Find Your Style challenge to get started with your style journey. https://40plusstyle.com/join
You took the words right out of my mouth.
Lol these commenters. How sad do you have to be to brag in a comments section on a style blog about how men won’t date you bc you look too young. I mean that is def not even a thing unless you look 14.
No matter how you feel, don’t ever put yourself down. There are plenty of us large girls, never fear. Think about who you are trying to please when you pick your clothes. If you haven’t had a season of your life when it’s all about you, what’s the risk in deciding to explore that? There are a lot of negatives to getting older but the big benefit no one discusses enough is freedom!
You will feel it, the lessening of a desire to fit in perhaps or the nagging voice that says wow, look at those purple heels, who am I trying to please by ignoring what I find exciting? My Dad always said the best thing about being old is he could say whatever he wants and get away with it. I feel like the same applies to clothing. Take one day a week and find stores you’d never shop in, either their look is way too young, way too inappropriate for your body style or confidence–those not in a million years places. Think of it as a ridiculous fun night where you get to try on and laugh at all the most bizarre things, just you and a dressing room. These are my favorite days and oddly enough, I always come out reinvigorated and not at all ashamed. You will learn some amazing stuff too, find things you can wear that you never would have tried on before or discover some really juicy stuff. For me, I was told I was fat as a child and spent most of my life using clothes to hide and keep people from looking at me (because I didn’t want to look at myself!) Then one day, the lady who writes this sent me a body type quiz, I found out I had an hourglass figure, and was a crying wreck for a whole week because what I was supposed to dress like broke every single rule of fashion I’d been taught. What could I do? Me and a dressing room date of absurdity every week helped me embrace the idea that it’s ok to say whatever I want and get away with it, because I am learning to wear what I want to say and having a blast. That’s what age gets you and don’t let anyone take that away from you!
I am 48 years old and I personally disagree with several things in this article. Plus this article is only someone else’s opinion. Plus I am a non-conformist.
Some of us who are in their 40s do not look like we are in our 40s. I personally love to show off my belly. Plus I do not like wide legged jeans or flare jeans. I do not like anything that is baggy. I like tight straight legged jeans and there is nothing wrong with high waisted jeans depending on the brand and the cut. I still wear some designer jeans from the 80s and I still look hot in them.
And btw, can we please stop referring to high waisted jeans as “Mom Jeans”? I personally find that term offensive, degrading, and stereotypical. How about we just call them “jeans” or “high waisted jeans”? It just amazes me how society allows a Television Program like “Saturday Night Live” and the media to influence our fashion decisions.
My advice is to wear what you want to. Especially if you look good in it. Who cares what someone else thinks?
The “SNL” bit on “Mom Jeans” is hilarious.
I do on occasion like to show a little bit of belly when I’ out. I like to show off my belly at the gym and of course when I’m at the beach.
Omg I couldn’t agree more I am 38 years old and am told I look in my 20’s I will dress how I want if I feel good in it. I address with confidence.
Preach, sista! Love it.
Thanks for your post.
I was wondering what you think about the “lace”, I personally love the lace.
What would be the guidelines to use for example a lace blouse?
Thanks!
yes lace can be fabulous. i personally feel that lace works best when the design is quite fine and intricate. Something like this blouse https://rstyle.me/n/cw4cebcmww Of course you need to make sure that there is enough coverage underneath, preferably in the same color.
Why do I have to avoid ripped jeans if they are ripped in the right spots? LOL. I’m 40 but i don’t feel or look like it. I feel like a couple of rips on the knee isn’t so bad.
It’s only a guideline. If you love ripped jeans, go for it! Certainly now that ripped jeans are very much in style.
My experience has been that women (well, men, too, but that is not the topic) either have a sense of what looks good on them or they don’t. They either have an “eye” or they don’t. I can’t tell you how many women I know who “think” they look fabulous, whereas my opinion is otherwise. And so many women take on trends just because they are trends, and do not take into consideration whether those trends are flattering on them!
I recommend to all women who are not confident in their own ability to choose what looks fabulous on them that they ask a friend or relative who always looks fabulous to act as their stylist. Of course educating oneself on what styles are most flattering on one’s body type is useful, but it is only in putting on different clothes and determining what works for one’s body that true discernment develops.
I also think it is funny when women say, “If you are over forty, you should not wear tight, ripped jeans, stilletos, too-tight plunging necklines, etc., etc., as if those looks are flattering on ANYBODY of any age! Ugly is ugly, unflattering is unflattering, and women of all ages and all body types make very wrong choices in an effort to be trendy.
In my opinion, classic, flattering clothing ALWAYS wins over unflattering trendiness, and a woman in unflattering clothing is never stylish. And of course women are absolutely free to wear whatever they like! But LIKING a look does not inherently endue upon it the title of “flattering,” nor does “trendiness” or “hipness” necessarily equal true style.
Yes it’s absolute true that some women have an innate sense of style while others don’t. But I disagree with you that style can’t be learned. I have seen amazing improvements from the women in my programmes. Of course improvement only comes through practise as you also mention which is why we do a lot of that in the privacy of our own community. The style club in combination is truly a great combination as it allows you to learn how to style yourself for your unique style and body type step by step, while at the same time getting immediate feedback from friends in the community. I talk more extensively about this topic at https://40plusstyle.com/style-can-be-learned-dont-believe-anyone-that-says-otherwise/
Everytime I search for the right tunic to wear with leggings…it never seems to feel right on me. I feel like it’s too baggy or even cold feeling. I live in a ski mountain resort city and winters here are chilly. I love leggings though, because they are so warm…and tight tops don’t really go with them, but geez they do feel warmer than billowy baggy like tunics. I don’t know but I feel like I look like Ms. Potato Head when I wear these two combinations.. Ha Ha!
I have more tips for wearing leggings and some of my own examples at https://40plusstyle.com/how-to-wear-leggings-over-40-an-extensive-guide/
I have a trick for tunics that works well for me in winter months. I layer a shorter sleeve or sleeveless billowing tunic from the summer months with a cropped wider type sweater. Off the shoulder crops especially look cute if the tunic is sleeveless. It breaks up the Length so as not to look like it’s pulling you down. Also helps with warmth.
What about bikinis?
I’ll be 40 next year and I’m not ready to give up wearing bikinis just yet. I’ve still got my bikini body and since I’ve never had kids (and don’t intend to) I’ve never had stretch marks, etc.
I don’t see any reason to ever give up bikinis. I still wear them 🙂
Hi could you tell me where I can find this fantastic long white sleevless shirt? It’s perfect!
https://40plusstyle.com/wp-content/uploads/2011/08/howtodressafter40.jpg
The vest is from Stella Carakasi. You can find winter versions of this vest at http://bit.ly/1ZVB7nf
Hi ladies. I’m a 52 year old woman stick in time. I tries to keep up with the trend but feel out of place. I don’t know where to start nor how to begin. Please help
Well there are now 1200+ articles on this site to help you on your way. You can start by visiting the start here tab at the left. However, the best and quickest way to really discover and jumpstart your style is my style course which you can find at http://40plusstylecourses.com/course/21-steps-to-a-more-stylish-you/
I’m 44 and love fashion, l tend to dress with a little edge , I have a pair of black over the knee boots that I absolutely love, I hope they are age appropriate.
If you feel fabulous and confident in them, then they are!
Thank you so much! I recently lost 100+ pounds very quickly due to complications from an accident…and turned 55.
It’s been tough breaking out of the dark colors and shapeless/frumpy mindset. And, it will take some time and hard work to stop looking like a deflated Dr. Seuss character.
I’ve been concerned that the excitement of choosing new styles will seriously blur the line between tasteful and age-appropriate. I can’t begin to describe the difficulty finding sites that don’t cater to teeny-boppers; or for mature women that don’t place an emphasis on crisp and professional. I work as a writer for various charities in a home office. Of course, I want to look semi-polished. But, I have no need or desire to be fussy about my appearance every day.
The advice and pictures you’ve offered are infinitely helpful! Thank you again!
Thank you Becky. Great to hear that you are having fun with style again. There are more than 1000 articles on this site and many more pictures so I encourage you to browse the archives for lots more inspiration and tips!
I wonder what Anna Wintour, Anna Dello Russo, Corine Roitfeld, and Donatella Versace would say about this list. They are all in their 50s and 60s and are all my style icons except for Donatella. Corine and ADR are the ones I emulate the most because we share the same fashion sense except my legs aren’t as thin as theirs, I don’t feel comfortable wearing short skirts and dresses, and up-to-there slits. Oh and sometimes ADR’s style leans towards the fantastical (she likes to make an entrance).
Bottom line is that we should all wear what makes us feel good and fabulous. That is the ultimate style rule!
I’m nearly 41 and wear mainly skinny jeans and loose tops I’m 5’8 and a size 12uk would you say I’m too.old for skinny jeans?
I don’t think you are ever too old for skinny jeans!
Hi, I am 45 years old and live in Phoenix where it is HOT for many months out of the year. I have always been a t shirt and shorts kind of person but now I feel very aware of how I look in those shorts (which isn’t terrible, just not like I was 25). What are your thoughts on shorts for the hot months and what length do you suggest? Thanks!!!
If you feel happy, beautiful and confident wearing shorts, wear them! You can pull off any look so long as you are confident about wearing it. However, if you start having doubts about any of these it will show. As for length it really depends on what you are wearing with the shorts. Creating a nice balance and silhouette is key here.
Thanks so much Sylvia! I am pretty comfortable with shorts just above the knee. I just didn’t want to wear anything that made me look too much like my teenaged daughter or anything that is too old for me. I really appreciate your feedback and I love your website! The visuals are great for someone like me.
Sylvia’s guidelines are a great resource in an era when women are confronted by so many style options. Confronted by so much choice, it can be difficult to develop a unique personal style the way iconic women like Jackie Kennedy and Grace Kelly so convincingly did. But breaking the fashion rules is important because when a woman wears what’s unexpected she demonstrates a fearlessness that’s both empowering and engaging. She’s being true to her own unique style.
Oh I love wearing ripped jeans. And if you pair them with a nice classy sweater or coat it will totally created the best effect. xo Sabina @Oceanblue Style
What a fantastic site! Thank you so much for the guidelines which are there for us to consider for our individuality and personal world. I appreciate it. I have found lately that I’ve got better at the science of working out lengths of tops and bottoms, which height of boot looks best with what and which length of necklace works. I too have been told I look a fair bit younger than my age (mid forties) but still work hard not to dress too young but classic with a hint of chic. I especially love leggings and will be very sad when/if they go out of fashion. Thanks again.
Thanks for your kind feedback Jayne. Enjoy browsing the site! 100s of articles for you to enjoy…
Dear Silvia, I also am not a type for guidelines and also dont think it has got anything to do with age at all. I personally feel that there is still a lot of tolerance missing in public opinion. But sharing ideas I find most inspiring. So I would really appreciate your input on my gray-in-gray with white blouse combination! Thank you.
Lovely layering outfit Sabina and love the grays together!
I think this can apply to someone from late thirties and up. I see a lot of women around 39 that dress like teenagers.
So what if some women who are over 39 dress like teenagers? If they can pull it off then I say let them.
I really hate it when someone decides that their fashion sense is “the only fashion sense”. Telling people over 40 they shouldn’t wear this or that… Just because you are old and maybe look old, doesn’t mean that all women over 40 appear old, wrinkly and have one foot in the grave. I don’t dress like a 20 year old but dress classy (my friends who are politicians, Dr’s and fashion designers…say so anyway) and am constantly asked my advice on fashion. I just tell people to wear what makes them happy. Most people don’t dress (in my circle anyway) like the “before” on makeover shows on tv, they dress like the “after”. If I want to wear a pair of ripped up jeans, I will. I have a great body, look in my 30’s (I’m not in my 30’s and haven’t been in more than a decade) and when people see photos of just my face, they are shocked that I am my age. I like to wear a more natural make up, my hair more simple and not colored. I am a vegan and take care of myself, don’t drink alcohol, don’t smoke, never did illegal drugs, exercise. SO my advice is that you can wear ripped up jeans if you want and the occasion warrants it (a rock concert maybe?) Maybe don’t wear them to the Opera lol. But it’s up to you to do what you want. People need to be themselves, not try to be what someone else teaches. I have read so many fashion magazines, blogs, watched tv shows, etc. They ALL give different advice on the exact same thing. Fashion isn’t a science, ladies. It is individual. Be yourselves. Who cares if someone else likes it or is jealous of it (of course when people tell me how they love the way that I dress, I do enjoy it). Live, Love, Laugh… and dress for your wants and needs!
I agree with a lot of what you are saying. And there are quite a few articles on this site that give exactly that message. We also sometimes have some lively discussions! Still, quite a few women like some guidelines and that is what I have given here in this article. Feel free to ignore them as you please. I wholeheartedly agree with your last sentence!
Sylvia seems to be a caring person and her guidelines are helpful for many women.
Since you seem to have all the answers you need, perhaps you could start your own site to share your fabulousness?
Sound advice! Thanks so much.
Great site and sound tips.
Sorry, But I love mom jeans. I grew up wearing low rise jeans. But I am very drawn to high rise jeans, especially vintage ones, like “mom ” jeans. I also like cut off shorts. And i like ripped denim. I love white button up shirts, and white t shirts. I have white t shirts in cotton, silk, and even soft leather. I like macthy match. Of course there was none of that when I was younger. But now at thirty, i want things to match. i LOVE wearing a top and skirt in the same pattern. So chic. Maybe I’m just not ready to grow up.
Good for you Martine! Ultimately you must do what makes you happy. Anything I say are just broad guidelines that you can choose to ignore.
Martine, you shouldn’t have to say sorry to anyone for wearing what you like, life is hard enough without the added stress of having the dress police on our backs!
Hi Sylvia,
Your readers are in good hands. It’s difficult to find style and fashion advice for women over 40 that I agree with 100%. As a certified personal image consultant and wardrobe stylist, most of my clients are women over 40 who ask similar questions as your readers. So glad they are getting terrific suggestions and pointers to express themselves by choosing styles that they love to give them pop and polish.
Best wishes for much success.
Marian Rothschild
I totally agree!!! Im 42 going to be 43- I look good, especially for my age! who says disressed jeans or skinny jeans are for teens? Even the concert T shirts that are out are music from my generation lol and these kids are wearing them but if I wear one someone may say Im trying to hard to be young. Live life to the fullest… be yourself and wear what you want as long as it makes you happy. I am not ready to shop at coldwater creek
If you have great legs, shorter length shorts are fine.
I think the most essential thing is to count on the expertise of 20-something clerks in women’s clothing stores. If one of them tells you that a piece of clothing makes you look “young and hip”, you should definitely buy it.
Unfortunately not all shop assistants are experts though and many will say anything to sell an item. You will still need to trust your own judgement and go with your instinct.
I don’t count on the “expertise” of the 20 something or any other age sales assistant!
I look at three things:
1 – Do I like it?
2 -Does it look good on me?
3- Will it make the “age appropriate” dress police enraged?
If it ticks all 3 boxes, then, I will buy it!
I do work out, diligently, have been doing so for about 3-4 years, 5 times a week, weight training and bodyweight exercises, eat properly, I am 5.4, tall, weight 58 kg, wear size 6 US and have 18% body fat, which is regarded as lean. http://www.builtlean.com/2010/08/03/ideal-body-fat-percentage-chart/
My tummy is flat, I have visible triceps, quads and firm, rounded butt. I can bench press 40 kg for 10 reps, do about 30 push ups from toes, 12 parallel unassisted dips and 3 unassisted chin ups. In the fitness world my achievements are very modest/mediocre – nothing to crow about. However, how many 50 + women outside the fitness/gym environment to you know who train and perform like I do? Here’s my bench press video on FB: https://www.facebook.com/photo.php?v=552248608205736&set=vb.100002618040492&type=2&theater That’s 47kg for about 4 reps.
Back in 2010 my now ex husband has told me that I will quit in about 2 months! LOL
I’m impressed Helen. It looks like you are well on your way!
Thanks 🙂
I don’t give a f@#! about rules, I am over 50, work out, and wear what ever i like that looks good on me and those who don’t like it can kiss my firm and mascular glutes!
By all means Helen. These ‘rules’ are only there for those that like some guidance. You will find that we break these ‘rules’ frequently here at 40+Style and have lots of fun with style and fashion!
Helen, I am not even sure why someone would take the time to read an d reply to the article if they did not care about what they wore.
I’m 46. 5’4″ and I weigh 150. People tell me I look young. Which is a good thing. 🙂 What is a proper dress length just for casual days? I am very classic as far as style goes. Thank you
I wrote an article about skirt lengths that would apply to dresses as well. Although I personally prefer on top or just under knees slightly higher will work too. It comes down to your personal preference. https://40plusstyle.com/what-is-the-perfect-skirt-length-for-women-over-40/ When I’m on the beach or holiday, I tend to go shorter with my dresses.
I’m a rectangle so I looked at your suggested site Zara. Yuk! Most of those shirts and dresses look like G.C. Murphy and dime store (think Big Lots now) leftover rags from the 70s. Young models with bellies showing in short tops-cute for them but those items are not suitable for women over 40 even superfit women in shape. Get some real suggestions for us that will work so we don’t all go shopping and get something that “will do” but is not very attractive or flattering.
I offer suggestions all the time in the many articles already on the site. Fashion changes all the time, so if Zara had good things one season, they may not do so necessarily the next. Also, Zara is a shop where you need to be picky. A lot of things are for very young women, but I still use it as a go-to shop for myself as there are always things that are good for us too. If you want to read more suggestions for the rectangle visit this page: https://40plusstyle.com/how-to-dress-the-rectangle-body-shape/. I also have a page of other good shops for women over 40 here: https://40plusstyle.com/best-online-shops/ If you want to understand why we can’t feature only 40+ women in fashion posts, you may want to read this article: https://40plusstyle.com/fabulous-40-plus-women/
I am 42 yrs, I think I look like a barrel with 204 lb my burst 45, waist 43, hip49. I don’t know what to wear any more.
You can look good no matter what you body shape is Lena. Start with this article and find out your body type. Then follow some guidelines for your specific body type and start exploring! https://40plusstyle.com/how-to-determine-body-shape/
Hi Ms. Sylvia,
Thank you for these very helpful advises on how wear clothes. I have just bought these long maxi dress (46 inches long) from the net, I am 5 ft (152 inches) only. Please give me advise on how to wear this. Thank you very much.
Hi Adel. This question is also addressed at this article on how to dress when you are petite https://40plusstyle.com/how-to-dress-when-you-are-short-petite/
I abide by a few rules:
1) Wear trends/fads as accessories
2) Never too tight, too low or too much
3) Simple cuts and mostly solids
4) Don’t wear anything like a teenager or 20-something would
5) Hide your flaws, accentuate the positive
Some great rules!
Hello, I am 42 yrs old- can I wear cowboy boots with a dress, or is that too young?
Yes for sure. It’s not too young but I do think you need to be careful with styling them as they can have quite a wide fit over your calves which is not always a very flattering look.
I’m 46 and I wear cowboy boots with dresses almost every weekend. Or even with a jean skirt. I even wear red boots, green boots and multi colored boots…I wish I could upload some pictures. I do not agree that a colored cowboy boot after 40 is a no.
Hi Karen,
Tag me in the FB group 40+Style Community and I’ll post pictures there.
Awesome – thanks! 🙂
If you like cowboy boots with a dress and you think they look good on, go ahead and wear them 🙂
I have 3 rules about dressing:
1-Do I like it?
2-Does it look good on me?
3- Is it appropriate for the occasion? ( eg, job interview, BBQ, wedding, funeral etc)
If the answer is yes to all of the above, then I go ahead and wear it, with pride!
The person who came up with archaic age appropriate rules should be praying to god that I never find him/her!
I am 41 and I don’t feel like there are rules for dressing over a certain age, at least not yet 🙂 I think this post is PERFECT for most women.
I disagree – There are Rules for dressing you should follow when your over 40 – Im 46 – 5’10 1/2 and I find that if I wear certain clothes I can look like mutton dressed as lamb. I don’t wear mini skirts in public, I find myself dressing in black and nothing else. I have brought my FIRST EVER pair of fitted pants just below the knee. They look groovy with a my high heel ankle boot.
I would like to see more dressing for women who are tall.
There are some women like myself who have good figures who are not fat nd have legs like a teenager through good diet and exercise so we can wear what we damn well please without looking like an old bag before your time. Black saps the hell out of your complexion by the way!
Umm, Elaine, do you know Dee or what kind of complexion she has? Perhaps black is not a good color for you, but it works for many women.
And the whole purpose of this webpage seems to be to help women not “look like old bags,” so you aren’t wrong there!
Thanks Dee! I was starting to shrink in my seat reading these comments. I am 48 and in fairly good shape, I do daily spinning classes and weight training a couple days out of the week. My husband loves the way I dress. I feel comfortable in anything as long as my boobs aren’t hanging out. Fitted dresses, skirts, skinny jeans, and high heels are a big part of my wardrobe. The only thing I don’t like is mini skirts, but that’s been all my life, just not something I’ve ever been comfortable in. Oh, and I am a makeup addict, nothing crazy but I do love taking care of my skin and makeup is always a must for me. I must say that I do get the evil looks from other women sometimes and it does make me question myself. But then I look in the mirror and I get over it. 🙂
Jay I echo your sentiments. I am 50 and I am the same. I also wear skirts about 4” above my knees. A nice short tweed skirt with oversized cashmere sweaters and long boots is one of my favorite outfit this fall. Of course to each is own. Of your are not comfortable or confident in a specific stile or clothing then do not wear it would be my advise. I still wear my over knee Stuart Weitzman Hiline boots tasteful and also own Burberry trench and my Chanel double flap., my wardrobe staples remain classic timeless with an edge. Embrace your confidence ladies and showcase that in your wardrobe ensemble. Cheers!
Um…..?!
I’m 44 years old. I am 5’4″ and 102lbs. My stats are 32-24-33. My thigh is 17″ in circumference without a scrap of cellulite. My inside leg is 31″.
I live in southern California where it is hot hot hot all the time. I LIVE in my booty shorts and after 3 kids I am proud of it. The rules are: there are no rules these days except 1 golden one: look at what you have, and DRESS TO SUIT IT.
Fitted pants below the knee look awful on me. I’m too short. Bet they look amazing on Dee though at 5’10”. I can only get away with a long skirt if it is A line – otherwise I look like a southern belle toilet paper holder. Low waist skinny jeans with a flowy top and some heels and the right jewelry make me feel a gajillion dollars. My only nod to my age – if I wear my booty shorts, my top is loose and doesn’t show too much skin. If I wear a tighter, more revealing top – I cover my legs more.
We women can do whatever we want these days – as long as we work with what we have and keep it classy.
Amen.
I think fashion can still be fun and many of these rules (I still wear shorts and cutoffs when I dress casually. I’m 46.) are old-fashioned. Never been one for tacky clothing (bejeweled words, overly ripped jeans).
Again, common sense reigns.
These tips are very helpful. I am 44 years old and love love love fashion! i am constantly balancing my ever growing wardrobe to make my hubby happy (he likes jeans and a tight black t-shirt) and my love for trendy clothes along with my professional wardrobe. I realize that I can’t dress with the latest fads even though i would love to! I also love accessories and shoes but am realizing that I need to go with more lower heels now cuz my back can’t handle it anymore. I look forward to reading the rest of your blog.
Now onto finding what to wear for my body style… I am short (5’2″ and around a size 10 or 12P) and hourglass figure with a little of a tummy and bigger chest (36DDD).
Hi Kim, Glad that you enjoy my blog and find it helpful. For your body type you way want to have look at my article on how to dress when you are petite: https://40plusstyle.com/how-to-dress-when-you-are-short-petite/. I have yet to write an article about dressing for larger bust sizes, which I will do shortly.
Thank you so much for all this information. i need a wardrobe makeover and this has helped me a lot. I really appreciate it.
Thanks for your kind feedback Ruth!
Amazing information. Thanks Sylvia. I’m straight or banana type with 41 inches bust 36 waist and 42 hip. I’m 5 feet 6 inches tall. Please suggest what kind of clothes should I wear. I’m 40 yrs old.
Hi Vinita, Check out my article on How to dress the rectangle body shape. That should get you started.
some great tips here! My fear when dressing is that I’ll look like I’m trying too hard, or trying to look younger than I am. I think it looks terrible when someone my age or older is wearing, let’s say, really tight ripped up jeans and a top with a huge word boldly splashed across its front, and wearing it off of one shoulder….super high stilletos, gaudy jewelry and overdone makeup. It just looks pathetic, unfortunately. Luckily for me, that sort of look was never my style, even when I was a teen, so it’s not hard to avoid it. I still think about it though when I’m shopping or dressing….’is this age appropriate for me?’ I really want to remain playful and stylish, but I don’t grab just anything that catches my eye anymore.
Thanks Tracy. I think you can still look very hip and be very creative with your clothes over 40. But as you say there are some things that you can better leave to the younger generation…
I agree with Tracey I used to think when I was younger, when my older friends used to say I don’t wear things like that anymore ive already dressed like a teenager I am not an an age to do it again and it looks ridiculous. I would respond by laughing at them and saying who the hell cares. But now I am 41 I can see what they meant. And yes it does take me ages to find something to wear no because of not being able to just grab anything. Embrace your classiness , I still wear a leather jacket but I pair it with a blanket scarf and just little touches like that.
Hi my problem is I look very young for my age I’m 44, and still get away with younger clothes, problem is I know my age and want to dress more for my age I’m slim and height 5″ 5″ what do you suggest?
Chillout and pick something that you love. Then couple it with one of the great tips on this sight. Being pathetic is a state of mind, it’s not about what you have on. Sure… we all want to look our best and be relatively age appropriate, but that doesn’t mean there are any rules, just guidelines really. Consider this…
I have two beautiful sisters, one dresses in very youthful clothing, big jewelry, hair and makeup. She always has since her teen years.
The other sis dresses like she is old and tired and retired haha sorry Jes.
But they both have reasons for doing this, that I think are nuts, the one sis is so dreading getting old, She thinks the young looking clothes help…they don’t. Sorry sis.
My other sis so dreads looking tacky, aka (desperate)that she jumped off a frumpy cliff in the other direction. My advise, if anyone wants it…
Find a comfortable happy medium, with style. Be happy! don’t over think it…life is short. Just be you. Good luck to all.
Wow lots of comments here.
I have a question.
What is the brand of lace heel you are wearing with the green satin skirt?
Thank you
Those shoes are by Lisa Tucci (old collection though)